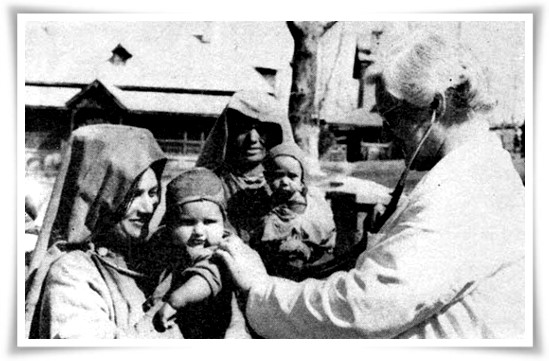
Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY) is a national public health insurance scheme of the Government of India that aims to provide free access to health insurance coverage for low-income earners in the country. Roughly, the bottom 50% of the population qualifies for this scheme. The Ayushman Bharat PM-JAY, launched on 23rd September, 2018 in Ranchi, Jharkhand by Prime Minister Narendra Modi, is the largest health insurance scheme in the world providing a yearly 5 lakh rupees cover and targeting approximately 50 crore beneficiaries of poor and vulnerable families; making up 40% of the Indian population. Rural households which are included (not excluded) are then ranked based on their status of seven deprivation criteria (D1 to D7). Urban households are categorised based on occupation categories.
Ayushman Bharat PM-JAY was launched as a step towards Universal Health Coverage (UHC); ensuring all people have access to quality health services – including prevention, promotion, treatment, rehabilitation, and palliation – without incurring financial hardships. The scheme provides coverage of all diseases/treatments in government and private hospitals in the country. It covers three key elements of health care: access, quality, and financial protection. Portability of benefits is a unique feature of AB PM-JAY which enables the beneficiaries to avail treatment at any hospital, empanelled under the scheme, across the country. Additionally, the successful implementation of the scheme is crucial to India’s commitment to achieving universal health coverage, a key health target in the Sustainable Development Goals (SDGs).
“There shall be no restriction on any family, based on strength or age, to avail the benefits from the scheme. And all prior health-related services will be covered under this scheme. The scheme will cover the cost of three days before a patient is hospitalised and up to 15 days after hospitalisation. In addition, the patient will also receive the cost of medicines,” the announcement was made during the launch of the Ayushman Bharat PMJAY scheme by Jammu and Kashmir Lieutenant Governor, Manoj Sinha.
About 24 lakh J&K residents have already registered for the scheme and thereby making 48 per cent of families eligible for benefits under the scheme. Official records suggest that J&K has received over Rs 109 crore from the central government for the implementation of the health scheme. The eligible beneficiaries can register for the scheme at any of the Union Territory’s five thousand Common Service Centers (CSCs) — up and working across Jammu and Kashmir — or empanelled hospitals.
Ten thousand free and cashless treatments worth ₹7.21 crore have been provided to eligible beneficiaries under the scheme in the first forty days since the launch of the scheme, according to official data. Besides, 10.77 lakh golden cards have been issued in addition to 12.90 lakh golden cards issued under AB PM-JAY. The evidence points to the fact that the scheme has shown promising results in Jammu and Kashmir. Effective participation of beneficiaries through door-to-door registrations supported by Common Service Centres and comprehensive awareness and outreach campaigns by the district functionaries helped the scheme gain and keep its momentum. About 65 percent of 85,689 treatments under the scheme have taken place at private hospitals of J&K, whereas the government hospitals have been catering to more than 90 percent of all inpatient services in the UT. This scenario has helped in supporting the private hospitals for providing inpatient services within its limitations.
The delivery of health cards and services under AB PM-JAY has been going on smoothly since the inception of the scheme, but the challenges remain. There is a long way to go to ensure access to primary and tertiary healthcare for all, irrespective of social status. It is recommended that policymakers focus on the following objectives to make the scheme more efficient.
(1) To deliver on the promise of the National Health Policy and ensure availability, access, and utilization of high-quality primary healthcare through government health services. It has been calculated that one-fourth to one-third of out-patient care is sought in government health facilities in urban and rural areas respectively. This was despite the availability of free or low-cost treatment for a wide range of primary care services at many facilities. Many people avoid availing public health services because of long wait times, poor quality of care, and high health worker absenteeism. And this only drives – poor and rich alike – to private hospitals for all of their health care needs. The government hospitals need to provide accessible and efficient primary care and integrate it with secondary care under AB PM-JAY.
(2) No insurance option is available for out-patient care, and therefore its inclusion in insurance policies, including AB PM-JAY, can help improve financial protection and increase access to health services. As a starting point, diagnostic services and preventive check-ups targeting common Non-Communicable Diseases (NCDs) should be included in the insurance package. The step will improve the chances of a complete cure, in addition to preventing cost escalation, by enabling earlier identification and management of NCDs. However, appropriate mechanisms will have to be designed to incentivize providers to focus on preventive rather than curative care.
(3) The high out-of-pocket prescription costs need to be addressed. Medicines account for 70 per cent of the total out-patient spending, more than twice that of consultation and diagnostic fees combined. Rationalizing the use of medicines and further increasing the provision of free medicines can significantly help reduce the financial burden of out-patient care. National Health Mission’s “Free Drugs and Diagnostics Services” initiative needs to be made more effective in line with the National Health Policy.
Notwithstanding the difficult geographical and political topography of the region, the AB PM-JAY scheme has benefitted many people in J&K. A long list of challenges surrounding the implementation of the scheme must be overcome to improve the access to healthcare in the region and promote the goal of universal health coverage. Therefore, there is a need to plan on how AB PM-JAY can be sustained in Jammu and Kashmir for the years to come and also how its role can be expanded under a responsive healthcare system.
Reference
What is Ayushman Bharat health insurance? All you need to know about what is covered, eligibility & more, Economic Times, September 23.
1 mn golden cards, 10k treatments in first 40 days of PMJAY SEHAT scheme in J-K – Hindustan Times
PMJAY Health Scheme|47.9 lakh health cards issued in J&K (greaterkashmir.com)



Leave a Reply
You must belogged in to post a comment.